How biomeds and ISOs hold together the U.S. healthcare system.

The patient arrives in a sweater with the hood up. Jeans. Heavy socks. Arms wrapped around arms or hands buried in pockets and shoulders tense, working to fight off the chills overtaking them on a beautiful summer day when it’s 82°F outside.
They have a loud, barking cough and a pressure in their chest. Breathing isn’t too hard yet, but it isn’t easy. It’s like walking up a flight of stairs, taking breaths through a plastic straw.
They’re older. Maybe 85. COVID-19 has a bad reputation with their demographic.
You assess them. When did their symptoms start? Who were they in contact with? What other symptoms are they experiencing? It’s COVID. You’re sure of it. You run the test anyway. Of course, you’re right.
The patient will need a ventilator. Maybe in an hour or two. You can’t quite say. Your hospital has more than a hundred, but only half work. And all of those are keeping other patients alive.
The ventilators in storage could be saving lives. They could save this life. But the parts to repair them weren’t available. For some of them, it’s a software issue. The hospital biomedical repair technicians (biomeds) who repair equipment in the hospital don’t have the right training and software license to clear the error code and restart the ventilator.
Or the original equipment manufacturer (OEM) can’t send one of their own technicians to repair it. There aren’t enough of them to go around. Plus, it’s a pandemic. The OEM won’t send its people into a hospital overflowing with cases.
The COVID-19 pandemic laid bare what biomeds and health care workers across the country thought for years. If medical devices can’t be repaired by the hospitals and clinics that own them, or by independent service organizations (ISOs) that fill in the industry’s service gaps, everyone loses. This patient is just one.
Content:
Your Right To Repair
The Right to Repair movement seeks to enshrine government legislation allowing consumers and businesses to repair their own consumer and commercial devices and equipment. It argues that anyone should have access to the OEM parts, manuals, and software needed to perform repairs. To fix the things they own.
It’s an ongoing disagreement between manufacturers, users, and the people who perform challenging technical repairs. Not just in medical devices - although infusion pump repairs and similar repair work is our business - but in every industry you can think of.

As of October 2021, the public has been granted permission by The US Copyright Office (USCO) and the Librarian of Congress to repair software-enabled devices under the protection of copyright law. For medical devices, this means biomeds maintain the right to get into any software-enabled device, like a ventilator or infusion pump, to obtain diagnostics and conduct maintenance or repairs.
But limitations still exist.
In the summer of 2021, farmers put John Deere under the legal magnifying glass after running into unusual software issues with their tractors. New tractor models won't start unless a technician clears out error codes - putting farmers at the whims of the manufacturer’s in-house repair capacity. The company said farmers would have everything they need to make the repairs themselves by 2021, but they don’t. And now at least 6 states are working to enshrine Right to Repair laws that will compel the OEM to cooperate.
Unfortunately, as of November 2021, those same farmers have made little to no progress with the laws surrounding their right to repair their tractors. John Deere maintains that farmers technically already have the right to repair their tractors, and that copyright blocks repair technicians from accessing the software. And of course, John Deere won’t give them the tools needed to fix it.
Apple built a hidden software lock into its iPhones in 2019. If your phone needed a new battery, it could only be an apple battery. And it could only be installed by an Apple technician.
Imagine you dropped your water bottle. Your favorite water bottle. It cracked on the side. But it’s made of polyethylene. So that crack isn’t the end of it. A minor repair and you can still have years of happy times together. Except the manufacturer:
- Doesn't allow you to repair it.
- Sends legal notices asking you to reverse the repair.
- Wants you to pay for specialized training every year to authorize your ability to repair...
- ...and so on.
Some OEMs are extremely forthcoming with repair manuals, parts, and access to training. Others are strongly opposed to your hospital’s ability to use its own materials on its own things. Until the law is in place and clear across the U.S., there will be a schism between manufacturers, patients, and users.
Learn more about the Right to Repair movement. Download the PDF Now!
Why Does It Matter To You?
Hospitals, clinics, family doctors, and other healthcare institutions have obligations.
- To provide the best patient care you can.
- To be responsible with your budget.
- To provide doctors, nurses, and support staff with the tools to be successful.

The Right to Repair gives you more choices.
More choices help save money and cut down-time waiting for the manufacturer’s technician. Maybe the best and fastest option for your medical device repairs is sending them to a local ISO, or bringing one of its specialized technicians in. Maybe it’s sending the device for off-site repairs. Maybe it’s paying for in-house biomed training so your skilled staff can perform the repairs repeatedly on multiple units.
Maybe waiting weeks or more for parts or repair technicians from the OEM isn’t possible.
More choices help you maintain your institutional values, like sustainability - repairing and maintaining equipment rather than placing it in the backroom.
Why Big Medical OEMs Don’t Support Right to Repair
In an article written for the Wall Street Journal Paul Giovanetti, president of the Institute for Policy Innovation, characterizes Right to Repair as an attack on American innovation and a threat to patient safety.
Some manufacturer equipment repair rates range from $600-$800 per hour and require a four-hour minimum.
He writes, “...forcing manufacturers to disclose their proprietary technologies would erode the incentive for innovation and endanger patients. Today the Food and Drug Administration (FDA) regulates and monitors medical-device safety. The FDA demands that original equipment manufacturers follow its guidelines regarding software updates, patches, and more-comprehensive repair jobs. The uncertified third-party service providers who would conduct repairs if these bills pass aren’t regulated by the FDA. There’s no assurance they will follow FDA standards.”
In the recent changes brought forth by USCO and approved by the Librarian of Congress, OEMs maintained that granting exemptions for circumvention on software-enabled medical devices is futile, as the public already has access to adequate authorized repair services for their medical devices. OEMs also argued that the public’s right to repair their own devices would:
- Interfere with manufacturers’ regulatory compliance obligations.
- Negatively impact the overall medical device market, since the proposed uses for the devices themselves are commercial in nature.
- Create cybersecurity risks.
So, the USCO’s Register of Copyright recommended a new exemption: enabling circumvention of technical protection measures (TPMs) that restrict access to firmware and related data files on medical devices and systems for repair and maintenance needs.
But more broadly, OEMs continue to argue that patient safety is the primary concern in their pushback against Right to Repair legislation.
Here's Why That's Not True
In 2018, the FDA dug into that claim. It explored the possibility that additional regulation on repair service providers could be a benefit to patients in healthcare across the U.S.
As the basis for its investigation, the FDA reviewed a comprehensive study from the Emergency Care Research Institute (ECRI).
In it, the ECRI studied more than 2 million device failure reports submitted to the FDA over the ten years. In those reports…

0.005 percent of failures could be attributed to service or maintenance issues
In its final report, the FDA Report on the Quality, Safety, and Effectiveness of Servicing of Medical Devices, the FDA said:
- “...the continued availability of third party entities to service and repair medical devices is critical to the functioning of the U.S. healthcare system.”
- “...the objective evidence indicates that many OEMs and third-party entities provide high quality, safe, and effective servicing of medical devices.”
How Exactly Do OEMs Impede Your Right to Repair?
Powerful equipment manufacturers use proprietary repair tools, software, and diagnostics to prevent third-parties from performing repairs.

They prevent access to repair manuals.
Biomeds have been informally sharing repair manuals and related documentation in online forums for years. According to a 2020 report titled Hospital Repair Restrictions from the Federation of State Public Interest Research Groups (U.S. PIRG), the inability to access manuals is so common that at least one biomedical engineering training program in the U.S. incorporates specific training to find the necessary service information.

They use copyright claims to discourage the sharing of resources.
In 2020, the website iFixit rolled out what it called the most comprehensive medical equipment service database in the world. Shortly after, iFixit was targeted with requests from manufacturers to remove repair manuals from its database.

They require all repairs to be done by their own technicians.
There are gaps in OEM repair networks that must be filled by in-house biomeds and ISOs. OEM technicians provide quality service. But they can’t meet demand. And hospitals end up waiting in line. When lives are at stake, that wait equates to tragedy.
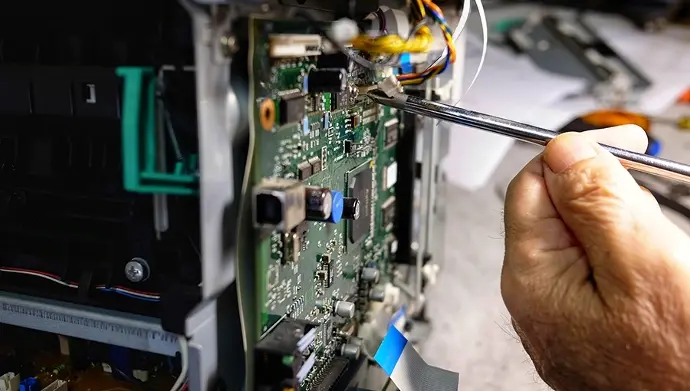
They use software to stop biomeds from working with their instruments.
Like Apple, many medical device manufacturers use software tripwires to impede your ability to repair your equipment. Removing screws from an ultrasound machine might trigger a software lockout, requiring an OEM tech to come reset the machine.
In May, the Federal Trade Commission completed a report titled Nixing the Fix. The report " identifies certain types of repair restrictions - for example, the use of adhesives that make parts difficult to replace, limits on the availability of spare parts, and the unavailability of diagnostic software - and examines the reasons manufacturers gave for those restrictions.”
Manufacturers, it concluded, were not well-founded in their explanations for repair restrictions.
In the PIRG report, almost half of the 222 biomedical professionals surveyed indicated they were denied access to necessary parts and information during the pandemic.
Even after the changes to copyright law in October 2021, strict limitations remain in place for possible exemptions made for repairing or diagnosing medical devices:
“Repairing,” “servicing,” or “maintaining” a device means restoring it to the state in which it functions in accordance with the OEM’s original specifications. OEMs make all of these processes nearly impossible by continuing to withhold parts and service manuals that allow a device to get back to its original specifications. This also leaves little room for making accessibility adjustments to devices.
Right To Repair: Federal And State
- In 2012, Massachusetts passed the first right to repair law. It requires motor vehicle manufacturers to provide the necessary documents to repair their cars.
- In 2020, Senator Ron Wyden of Oregon introduced the Critical Medical Infrastructure Right-to-Repair Act of 2020, removing barriers to fixing medical equipment during the COVID-19 pandemic, and for as long as the pandemic lasts.
- In 2021, 25 states have some form of Right to Repair legislation under review, including specific medical equipment right to repair bills in Texas (bill HB 2541), California (bill SB 605), and Hawaii (bill SB 760).
- And, in July 2021, in an executive order aimed at promoting economic competition, President Joe Biden asked the FTC to crack down on “unfair anticompetitive restrictions on third-party repair or self-repair of items.”
The European Union’s Medical Device Directive has required medical device manufacturers to provide service information since 1993. Not just on single devices where a supply issue was identified, but on everything. CT scanners, infusion pumps, fetal transducers, EKG monitors. The whole gamut of medical devices.
The pandemic pressure tested the medical device servicing system and exposed some key flaws. Ventilators were the story of the moment, but they’re a symbol for the entire medical device industry.

So, after the exemptions passed by the USCO, where do we stand with the right to repair?
The new rules don’t mean that OEMs need to make medical devices like ventilators any easier to repair. An OEM won’t give you the tools to crack open the back of a ventilator, nor will it give you the ability to access its software. But the rules give you the right to try.
We want to work with manufacturers to make sure patients are protected. That healthcare providers can be frugal, maintaining and repairing the equipment they own as they see fit. That we can reach a fair solution in this industry where innovation and cooperation help the whole system thrive.
The best way to ensure patient safety is to make sure equipment is being maintained regularly using the manufacturer's recommended procedures, and repaired using those same manufacturer-approved procedures. The only way to do that is if biomeds, ISOs, and healthcare providers have up-to-date manuals, access to parts and training, and the freedom to perform maintenance and repairs as healthcare systems need.
Want to learn more about your right to repair? Access the PDF anywhere, anytime by downloading a copy today.
Get Your Copy!
About the Author

Laura Collier
Laura Collier has a Bachelor’s Degree in Communications and a Master’s Degree in Business Administration from the University of North Florida. She is the Marketing Manager at AIV, Inc.
